<>
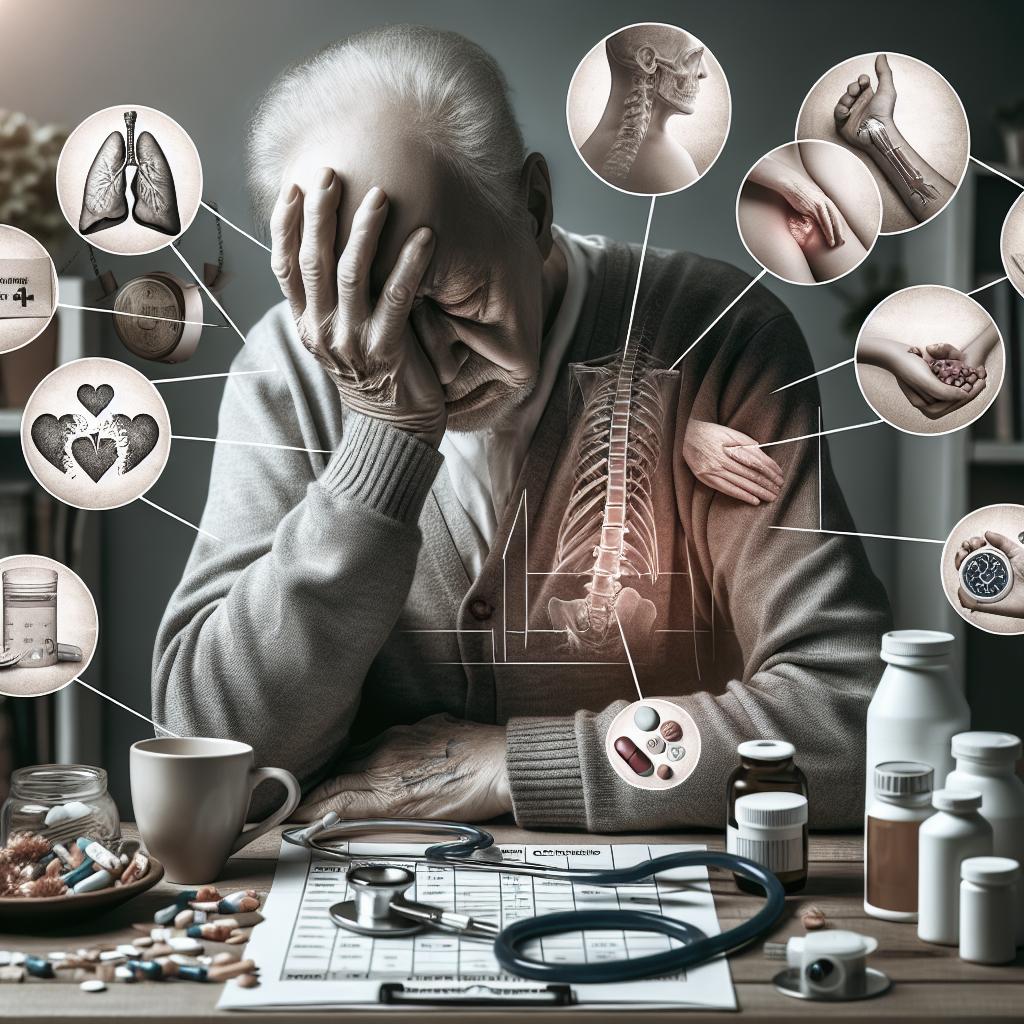
As our loved ones age, being prepared for the end-of-life phase becomes crucial to ensure their comfort and dignity. Recognizing signs of illness and understanding what lies ahead can provide caregivers with a sense of preparation. This article covers the timeline of end-of-life symptoms, specific physical and emotional changes, and ways to support your loved ones during this vulnerable period. We will also include lessons learned to encapsulate the key takeaways effectively.
End-of-life symptoms timeline
Weeks before end of life
In the weeks leading up to the end of life, elders often show notable changes in their daily routines. Their appetite decreases significantly, leading to weight loss. Additionally, they may have difficulty swallowing or show less interest in foods they once enjoyed. These changes are natural as the body begins to conserve energy for essential functions.
During this period, the elderly often experience increased fatigue. Their energy levels drop, causing them to sleep more and engage less in physical activities. This stage involves a lot of reminiscing, as well; they may frequently talk about the past or important life events, reflecting on their journey.
Days before end of life
As days approach, the signs become more pronounced. You may observe more significant physical weakness and an almost continuous state of sleep. The sleep becomes more profound and harder to wake from, and communication starts to dwindle.
Physiological changes such as reduced blood pressure, changes in breathing patterns, and cooling extremities are common. These indicate that the body is gradually shutting down. It is essential to ensure comfort during these final days through gentle touch and reassurance.
Hours before end of life
In the final hours of life, changes are even more evident. The skin may become blotchy, and breathing patterns may shift to irregular ones like Cheyne-Stokes respiration. These signs can be distressing, but are natural parts of the process.
The elderly may enter a semi-conscious or unconscious state, showing minimal response to stimuli. Keeping the environment calm and peaceful is crucial as they approach their final moments.
At death
At the moment of death, breathing stops, and there’s no response to visual or auditory stimuli. The body goes limp, and the skin may turn pale or bluish. Some may involuntarily release bodily fluids as the muscles relax entirely.
Though this is a difficult time, knowing what to expect can provide much-needed emotional grounding. It allows you to focus on ensuring a respectful and serene transition.
End-of-life symptoms
1. Appetite and digestive changes
Decreased appetite and changes in digestion are among the first signs of end-of-life. The body’s need for energy reduces, causing a natural decline in the desire for food and drink. Swallowing difficulties can also emerge, leading to a preference for softer foods or liquids.
In some cases, digestive discomfort such as constipation or bloating can occur. Providing small, nutrient-rich meals and staying hydrated can help manage these issues, ensuring they remain as comfortable as possible.
2. Sleeping more
An increase in sleep is common as the body starts to conserve energy for crucial functions. The elderly may spend more time in bed, showing a lack of interest in previously enjoyed activities.
It’s essential to support these sleeping patterns by providing a soothing and comfortable environment. Avoid waking them up unnecessarily, as rest is vital in this stage of life.
3. Withdrawal from the world
Often, the elderly will start to withdraw from social interactions and the world around them. This withdrawal is a part of the natural process of letting go and should be handled with sensitivity.
Respecting their need for solitude while providing presence and comfort helps maintain emotional stability. Continue to offer opportunities for social interaction without pressing them to engage.
4. Anxiety and depression
Mental health can deteriorate during end-of-life stages, with increased anxiety and signs of depression often emerging. It’s crucial to address these symptoms proactively through compassionate communication.
Offering emotional support and possibly involving a mental health professional can help manage these feelings, making the individual more comfortable during this challenging phase.
5. Urinary and bladder incontinence
As muscle control weakens, urinary and bladder incontinence become more common. This can be distressing for the individual and caregivers alike.
To manage this, ensure regular bathroom visits and use incontinence products to keep them dry. Creating a routine can help minimize discomfort and maintain hygiene.
6. Changing vital signs
Vital signs such as heart rate, blood pressure, and body temperature can fluctuate during the end-of-life period. An irregular heartbeat or labored breathing may become evident.
Monitoring these signs can help in anticipating the progression of end-of-life stages and managing any symptoms that cause discomfort, ensuring a peaceful transition.
7. Confusion
Confusion and disorientation are common as cognitive functions decline. The elderly may become forgetful or have difficulty recognizing familiar faces and places.
Creating a serene and familiar environment, and engaging them in gentle, grounding activities like listening to favorite music or holding familiar objects can help alleviate some of this confusion.
8. Sensory changes
Changes in sensory perception, such as diminished vision or hearing, can occur. The elderly may become less responsive to sights and sounds they used to enjoy.
Communicating through touch and reassuring words becomes increasingly important. Providing a calm, reassuring presence can help them feel secure despite these sensory declines.
9. Saying goodbye
Often, individuals may find comfort in saying their goodbyes. This can manifest as reminiscing about past relationships or leaving messages for loved ones.
Facilitating these interactions, whether through phone calls or written notes, can provide a sense of closure and emotional peace for both the individual and their loved ones.
10. Breathing changes
Changes in breathing patterns, including periods of rapid or shallow breaths interspersed with pauses, are common signs as the end draws near. This phenomenon is often referred to as Cheyne-Stokes respiration.
These changes can be distressing to observe, but they are a natural part of the dying process. Keeping the atmosphere calm and perhaps playing soothing music can help alleviate distress.
11. Loss of consciousness
In the final stages, the elderly may lose consciousness and enter a coma-like state. This is often a sign that the end is near, and responses to external stimuli diminish significantly.
During this time, providing comfort through gentle touch and a peaceful environment is vital. Reassure them verbally, even if they seem unresponsive, as the sense of hearing is one of the last to fade.
How to support your loved ones during end of life
Providing physical comfort
Physical comfort becomes paramount during end-of-life care. This includes managing pain, ensuring cleanliness, and addressing physical discomforts such as positioning in bed.
Regularly clean and moisturize their skin to prevent bedsores, and provide gentle massage to alleviate stiffness. Simple actions like adjusting bed positions to avoid pressure points can significantly enhance their comfort.
Providing emotional comfort
Emotional support is crucial as many may experience fear, sadness, or anxiety. Engage in meaningful conversations, offer reassurance, and respect their needs for solitude or companionship.
If possible, involve friends, family, or spiritual advisors who can provide comfort through presence and shared memories. Emotional connections can offer immense solace, both for the individual and those around them.
Lessons learned
| Stage | Signs | Support Strategies |
|---|---|---|
| Weeks before end of life | Reduced appetite, increased fatigue, communication | Offer small meals, ensure rest, engage in reminiscing |
| Days before end of life | Increased sleep, physical weakness, reduced interaction | Maintain comfort, offer gentle reassurance |
| Hours before end of life | Altered breathing, semi-conscious state | Keep calm environment, provide physical comfort |
| End-of-life symptoms | Appetite changes, sleeping more, withdrawal, anxiety | Healthy diet, support rest, respect need for solitude, emotional support |
| Support | Physical and Emotional Comfort | Manage pain, cleanliness, offer presence and reassurance |